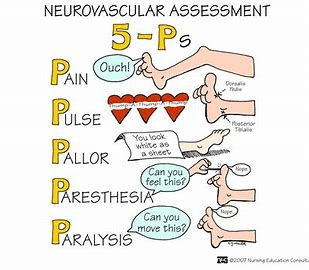
Risk factors for compartment syndrome trauma, plaster cast, ortho postops, burns, infected limb Osteoporosis and falls Risk factors for hip fx surgical fasciatomy fat particles lodge in vessel fascia can't expand to increased pressure Pulse use a doppler if you can't palpate this Pallor sign of arterial insufficiency below level of injury Paralysis Late sign of prolonged nerve compression or muscle necrosis This traction has an external pin distal to stabilized area 85% % of hip fractures in people older than 65 Buck's traction age, type of fx, bone quality factors considered for hip fx treatment neurovascular assessment focus areas (5Ps) aspirin, SCDs, TED hose lovenox DVT prophylaxis out of bed This should happen on post op day 0 1-3 days after injury (usually femur) when trauma pt will typically develop fat embolism neurovascular assessment assessing nerve function and blood flow to injured extremity This should never be placed under the knee after TKA Early mobilization decreases mortality rate after ortho post op something to reduce risk or hip fracture Pain Worry if this is out proportion to injury - - not relieved by meds ORIF open reduction internal fixation BKA below the knee amputation Paresthesia decreased sensation, hypersensation - result of nerve compression Risk factors for compartment syndrome trauma, plaster cast, ortho postops, burns, infected limb Osteoporosis and falls Risk factors for hip fx surgical fasciatomy fat particles lodge in vessel fascia can't expand to increased pressure Pulse use a doppler if you can't palpate this Pallor sign of arterial insufficiency below level of injury Paralysis Late sign of prolonged nerve compression or muscle necrosis This traction has an external pin distal to stabilized area 85% % of hip fractures in people older than 65 Buck's traction age, type of fx, bone quality factors considered for hip fx treatment neurovascular assessment focus areas (5Ps) aspirin, SCDs, TED hose lovenox DVT prophylaxis out of bed This should happen on post op day 0 1-3 days after injury (usually femur) when trauma pt will typically develop fat embolism neurovascular assessment assessing nerve function and blood flow to injured extremity This should never be placed under the knee after TKA Early mobilization decreases mortality rate after ortho post op something to reduce risk or hip fracture Pain Worry if this is out proportion to injury - - not relieved by meds ORIF open reduction internal fixation BKA below the knee amputation Paresthesia decreased sensation, hypersensation - result of nerve compression
(Print)
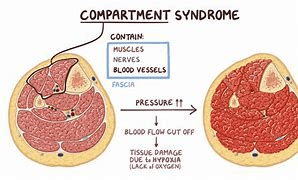
B-trauma, plaster cast, ortho postops, burns, infected limb
B-Risk factors for hip fx
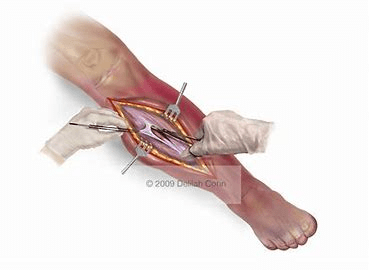
O-surgical fasciatomy
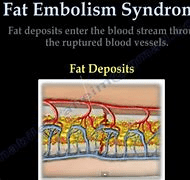
B-fat particles lodge in vessel
B-fascia can't expand to increased pressure
G-use a doppler if you can't palpate this
G-sign of arterial insufficiency below level of injury
N-Late sign of prolonged nerve compression or muscle necrosis
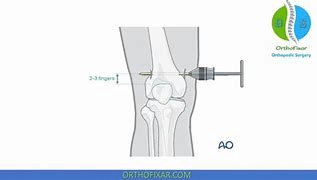
N-This traction has an external pin distal to stabilized area
N-% of hip fractures in people older than 65
G-Buck's traction
B-factors considered for hip fx treatment
I-neurovascular assessment focus areas (5Ps)
O-DVT prophylaxis
O-This should happen on post op day 0
G-when trauma pt will typically develop fat embolism
O-assessing nerve function and blood flow to injured extremity
G-This should never be placed under the knee after TKA
I-decreases mortality rate after ortho post op
O-something to reduce risk or hip fracture
N-Worry if this is out proportion to injury - - not relieved by meds
I-open reduction internal fixation
I-below the knee amputation
I-decreased sensation, hypersensation - result of nerve compression